Invited Symposium: Behaviour-Induced Neural Events after Brain Injury
| INABIS '98 Home Page | Your Session | Symposia & Poster Sessions | Plenary Sessions | Exhibitors' Foyer | Personal Itinerary | New Search |
Introduction
Traditional views of recovery of function following brain injury have focused on the influence of neuroplastic events on behavioral outcome. We have previously shown that the opposite is also true. Manipulation of motor behavior after brain injury can modify mechanisms associated with neuroplasticity as well as with neuro-degeneration and functional outcome. Extreme forced motor therapy of the affected forelimb, but not the unaffected forelimb, during an early critical period results in gross exaggeration of the original neuronal damage as well as in retardation of functional recovery following focal unilateral electrolytic lesions (Kozlowski et al., 1996) and fluid percussion injury (Kozlowski et al., 1996) of the sensorimotor cortex in rats.
Though it has been demonstrated that use-dependent exacerbation of injury occurs in lesion models involving mechanical injury, including deafferentation in electrolytic lesions as well as shearing and compression in fluid percussion injury, it is not known if it will occur in animal models of ischemic stroke or Parkinson's disease, both of which involve neuronal damage involving complex biochemical cascades in the absence of mechanical injury. Stroke is the major cause of adult disability in the United States. The ischemic cacade begins with a decrease in ATP production resulting from loss of energy substrates, and a subsequent failure of the normal membrane potential (Siesjo, 1984). Membrane depolarization triggers changes in calcium homeostasis through multiple mechanisms including NMDA receptor activation (Choi, 1992). Experimental middle cerebral artery occlusion (MCAO) in the rat mimics one of the most common of ischemic strokes occurring in humans, and preferentially damages tissue in cortical regions including sensorimotor and primary motor cortex. Parkinson's disease is the third most common neurological disease and is characterized by a loss of dopaminergic neurons in the basal ganglia, accompanied by akinesia, rigidity, and resting tremor (Conford, Chang & Miller, 1995). Infusion of 6-OHDA into rat substantia nigra preferentially destroys dopaminergic neurons, and leads to Parkinson-like deficits in rats. The present studies investigated the effects of forced motor therapy, by means of one-sleeved plaster of paris casts (Jones & Schallert, 1994), on anatomical and functional outcome following both MCAO and 6-OHDA infusion in rats.
Materials and Methods
Animal preparation
Adult male Long-Evans rats were used. Animals were food deprived for 12 hours prior to surgery and were maintained at 37° for all surgical procedures.
90 min 2 Vessel Occlusion (2VO)
Animals were anesthetized with chloral hydrate (49 mg/kg IP). The left middle cerebral artery (MCA) was exposed by drilling through the squamous temporal bone midway between the right eye and ear. After incision of the dura mater, a wire occluder (.005”) was introduced under the MCA, lifted gently, and turned 90°. Interruption of blood flow was confirmed using a Laser Doppler Flowmeter (LDF). The ipsilateral common carotid artery (CCA), which had been isolated via a neck incision, was occluded using atraumatic aneurism clips. At the end of the 90 min ischemic period, blood flow was reestablished and confirmed with LDF. Animals were casted for either:
30 min 3 Vessel Occlusion (3VO)
Anesthesia and surgeries were performed as for 90 min 2VO, but the left MCA and both CCAs were occluded. Blood flow was reestablished at the end of the 30 min ischemic period and confirmed by LDF. Animals were casted for 10 days and sacrificed at 32 days.
6-OHDA infusion
Animals were anesthetized with Equithesin (.035 ml/kg). 10 µg 6-OHDA (2.5 µg/ml in 0.1% ascorbic acid) was infused throgh a cannula into medial forebrain bundle using the coordinates of Paxinos and Watson: A/P -3.3; L/M +/- 1.7; D/V -9. Animals were casted for 7 days and sacrificed at 60 days.
Casting procedure
Prior to recovery from anesthesia, animals were either fitted with one sleeved plaster casts, as shown in Figure 1, or left uncasted. The upper torso was wrapped in soft felt, and the ipsilateral forelimb was wrapped in felt and positioned in a naturally retracted position against the animal's sternum. Plaster of paris strips were then wrapped around the immobilized limb and upper torso.
 Fig. 1: Rats were fitted with one-sleeved plaster of Paris casts.
Fig. 1: Rats were fitted with one-sleeved plaster of Paris casts.
Behavioral Tests
Forelimb placing
Each animal was held by the torso with forelimbs hanging freely. Contralateral and ipsilateral placing was induced by gently brushing the respective vibrissae on the edge of a tabletop 10 times. Contralateral results are shown (ipsilateral placing was 100% for all groups) as percent successful placing (number correct x 10).
Footfault
Each animal was placed on an elevated grid for 2 min. Each time a paw slipped through the grid, as the animal explored, a footfault was scored. Total number of steps was also counted. Footfault index was computed as (ipsilateral faults - contralateral faults)/(total steps). A score of 0 = no asymmetry.
Limb use asymmetry
Each animal was placed in a clear glass cylinder for 5 min and videotaped. Videotapes were analyzed in slow motion, and scored for placement of forepaws against the side of the cylinder as the animal reared. Ipsilateral, contralateral and simultaneous placements were tallied. Limb use index was computed as (ipsilateral - contralateral)/total. A score of 0 = no asymmetry.
Apomorphine rotation
Apomorphine (.25 mg/kg in 0.1% ascorbic acid) was injected subcutaneously. Animals were returned to their home cages, and contralateral turns were tallied for 90 minutes.
Histology
Forced motor therapy resulted in an increase in infarct volume following 90 min 2VO, as can be seen in Figure 2. Infarct volumes were larger in rats casted for 3 days and sacrificed at 3 days (A) and in rats casted for 14 days and sacrificed at 28 days (B).
Forced motor therapy resulted in exaggerated behavioral deficits following 30 min 3VO, as can be seen in Figure 3. Rats that had been casted were more impaired in forelimb placing (top) and footfault (bottom) than uncasted rats or shams.
Forced motor therapy resulted in fewer apomorphine induced contralateral rotations in 6-OHDA treated rats, as can be seen in Figure 4.
Forced motor therapy resulted in decreases in spontaneous limb use asymmetries in 6-OHDA treated rats, as can be seen in Figure 5. Rats that had been casted were similar to sham controls.
As can be seen in Figure 6, there was a significant relationship between spontaneous limb use asymmetry scores and dopamine depletion, as determined by tyrosine hydroxylase levels, in 6-OHDA treated rats.
Forced overreliance on the impaired forelimb has previously been
shown to exaggerate neuronal injury following electrolytic lesions of the cerebral cortex (Kozlowski et al., 1996). The results of the present study suggest that functional outcome following forced use of the impaired forelimb depends on the model being studied. If forced use follows focal cerebral ischemia, the volume of the infarct is increased and behavioral outcome worsened. In contrast, forced use appears to be benefical following a 6-OHDA dopamine lesion of the medial forebrain bundle (MFB), increasing dopamine levels in the striatum as compaired to lesioned animals not forced to use the impaired forelimb and dramatically decreasing behavioral deficits.
The difference in the effects of forced motor rehabilitation are
likely due to differences between these two models of neural degeneration. Tandem occlusion of the left MCA combined with occlusion of the left CCA resulted in ischemic damage to the cerebral cortex. Forced motor therapy directed at the contralateral forelimb was begun after primary neuronal injury had already occurred, possibly exaggerating the cascade of neurodegenerative events leading to secondary injury, thus increasing infarct volume and worsening behavioral deficits. In contrast, injection of 6-OHDA into the MFB causes slow degeneration of dopamine terminals in the striatum. In this case, forced rehabilitation of the contralateral limb occurred during degeneration of the striatum, and may have preserved
dopaminergic terminals, thus decreasing functional deficits that would
ordinarily result from a 6-OHDA lesion.
Conclusions:
Results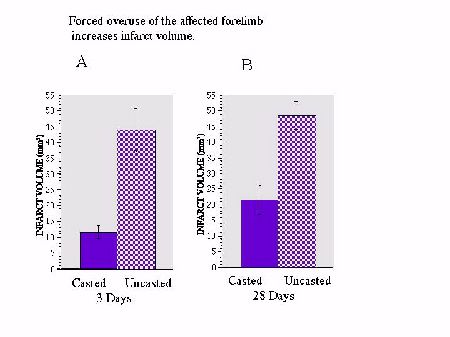 Fig. 2: Infarct volume 3 days and 28 days following 90 min 2VO.
Fig. 2: Infarct volume 3 days and 28 days following 90 min 2VO.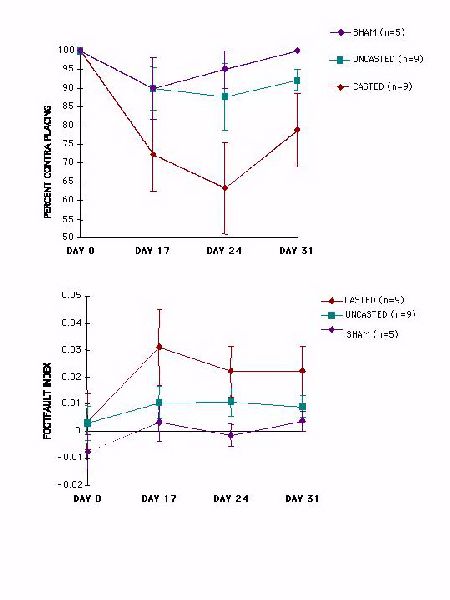 Fig. 3: Forelimb placing and footfault scores following 30 min 3VO.
Fig. 3: Forelimb placing and footfault scores following 30 min 3VO.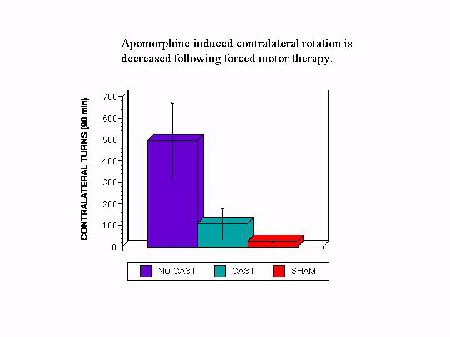 Fig. 4: Apomorphine rotation in 6-OHDA treated rats.
Fig. 4: Apomorphine rotation in 6-OHDA treated rats.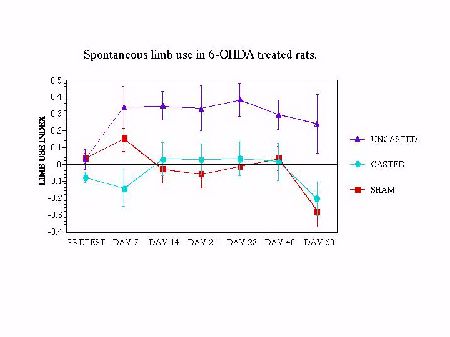 Fig. 5: Limb use asymmetries in 6-OHDA treated rats.
Fig. 5: Limb use asymmetries in 6-OHDA treated rats.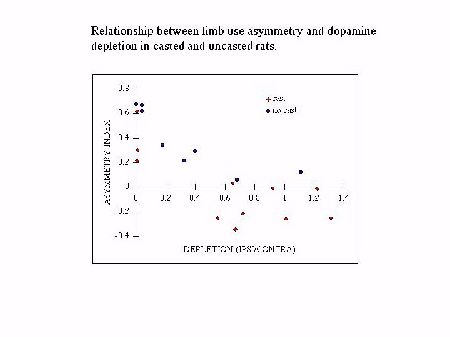 Fig. 6: Limb use asymmetries and dopamine depletion in 6-OHDA treated rats.
Fig. 6: Limb use asymmetries and dopamine depletion in 6-OHDA treated rats.
Discussion and Conclusion
References
| Discussion Board | Previous Page | Your Symposium |