Invited Symposium: Regulators of Skeletal Growth and Integrity in Health and Disease
| INABIS '98 Home Page | Your Session | Symposia & Poster Sessions | Plenary Sessions | Exhibitors' Foyer | Personal Itinerary | New Search |
Introduction
Vitamin D is critically important for calcium homeostasis and bone health. There are two sources of vitamin D. For most humans, the major source is exposure of the skin to sunlight (1). Vitamin D rarely occurs naturally in foods. However, some foods are fortified with vitamin D, and therefore, serve as a source of vitamin D. The major function of vitamin D is to maintain the blood calcium in the normal range. By accomplishing this, it maintains an adequate calcium and phosphorus in extracellular fluid that permits the normal mineralization of the skeleton. Vitamin D deficiency is now recognized as a major health problem for young children who live in countries where milk is not fortified with vitamin D, and in adults over the age of 50 years who are less active and do not consume food products containing vitamin D. Vitamin D deficiency can cause growth retardation and rickets in children. However, in adults, it has a much more subtle effect causing a mineralization defect leading to adult rickets and exace rbating osteoporosis.
1. Vitamin D
At the turn of the 20th century, rickets was common in industrialized cities of Northern Europe and North America (1). Vitamin D deficiency caused marked growth retardation and skeletal deformities of the skull and long bones. In adults, vitamin D deficiency has a more subtle effect on the skeleton. The mineralization defect resulting from vitamin D deficiency causes an increase in unmineralized collagen matrix (osteoid) known as osteomalacia. In addition, vitamin D deficiency-associated secondary hyperparathyroidism mobilizes precious calcium stores from the adult skeleton resulting in or exacerbating osteoporosis (2).
It is generally assumed that vitamin D deficiency causes hypocalcemia. However, this rarely occurs until the skeleton is so depleted of its calcium stores that it can no longer maintain normal serum calcium levels. As vitamin D deficiency ensues, there is a compensatory increase in parathyroid hormone. Parathyroid hormone goes to the bone to increase bone calcium mobilization and also interacts with the kidney to conserve precious calcium from being lost into the urine. However, parathyroid hormone also causes loss of phosphorus into the urine leading to low normal, or low fasting blood phosphorus levels. Thus, a low normal calcium with a low serum phosphorus level causes an inadequate calcium x phosphorus product to mineralize the collagen matrix (osteoid) resulting in a mineralization defect. This causes rickets in children and osteomalacia in adults.
2. Sources of Vitamin D
The major source of vitamin D for most humans is from their casual everyday exposure to sunlight (1). There are a multitude of factors that can suppress and even eliminate the skin’s production of vitamin D3. An increase in skin pigmentation or the topical application of a sunscreen will absorb the solar ultraviolet B photons thereby significantly reducing the production of vitamin D3 in the skin (3,4). Aging decreases the capacity of the skin to produce vitamin D3 because of the decrease in concentration of its precursor 7-dehydrocholesterol. Above the age of 65 years, there is a three to four fold decrease in the capacity of the skin to produce vitamin D3 when compared to a healthy young adult (5). The factor that has the most dramatic effect on the cutaneous production of vitamin D3, however, is the zenith angle of the sun. Thus latitude, season of the year, and time of day all affect cutaneous vitamin D3 synthesis (6). For example, in Bo ston, the zenith angle of the sun is at such an oblique angle in the winter that very few ultraviolet B photons (energies 290–315 nm) responsible for making vitamin D3 in the skin reach the earth’s surface. Therefore, little, if any, vitamin D3 can be made in the skin in Boston during the months of November through February. However, in Florida, the zenith angle if much less oblique throughout the entire year; and therefore, vitamin D3 production can occur throughout the year. As a general rule, latitudes above and below 40º north and south of the equator, respectively, significantly diminishes or completely eliminates the production of vitamin D3 in the skin during the winter (6).
It is principally oily fish such as salmon and oils from the liver of some fish such as cod liver oil and tuna that have adequate amounts of vitamin D. Liver from meat animals such as cows, pigs, and chickens do not contain vitamin D.
Several countries including the United States and Canada fortify milk with vitamin D. Some breads and cereals are also fortified with vitamin D. In Europe, margarine and cereals are the major foods fortified with vitamin D. However, some caution is needed regarding the use of these foods as a sole source of vitamin D. At least for milk in the United States and Canada, the vitamin D content was found to be highly variable. Approximately 50% of the samples contained less than 50% of the vitamin D that was stated on the label, and about 10% of milk samples did not contain any detectable vitamin D (7).
Synthesis and Metabolism of Vitamin D
During exposure to sunlight, the ultraviolet B photons with energies of 290-315 nm are responsible for converting 7-dehydrocholesterol in the epidermis and dermis into previtamin D3 (1)(Fig. 1). Previtamin D3 is unstable and undergoes a rearrangement of its structure within two to four hours to vitamin D3. Once formed, vitamin D3 selectively exits the epidermis into the dermal capillary bed where it is transported to the liver bound to the vitamin D binding protein. Vitamin D ingested in the diet is incorporated into the chylomicron fraction and is absorbed into the lymphatic system where it eventually is transported to the liver. In the liver, vitamin D receives its first hydroxylation on carbon 25 to form the major circulating form of vitamin D3, 25-hydroxyvitamin D3. 25(OH)D3, however, is biologically inert and requires an additional hydroxylation in the kidney on carbon 1 to form 1,25-dihydroxyvitamin D3 (8)(Fig. 2) . 1,25-Dihydroxyvitamin D3 (1,25(OH)2D3) is considered to be the biologically active form of vitamin D responsible for regulating calcium and bone metabolism. It accomplishes this by interacting with specific vitamin D receptors (VDR) in the intestine and in the bone. In the intestine, 1,25(OH)2D increases the efficiency of calcium absorption. In the bone, it interacts with osteoblasts and precursor cells of osteoclasts ultimately to mobilize calcium stores from the skeleton (8,9,10).
As can be seen in Figure 1.
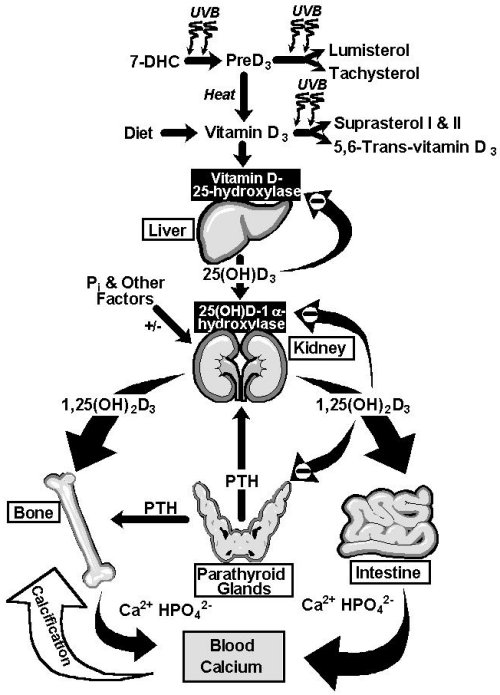 Fig. 1: Photosynthesis of vitamin D3 and the metabolism of vitamin D3 to 25(OH)D3 and 1,25(OH)2D3. Once formed, 1,25(OH)2D3 carries out the biologic functions of vitamin D3 on the intestine and bone. Parathyroid hormone (PTH) promotes the synthesis of 1,25(OH)2D3, which, in turn, stimulates intestinal calcium transport, bone calcium mobilization and regulates the synthesis of PTH by negative feed back (9)
Fig. 1: Photosynthesis of vitamin D3 and the metabolism of vitamin D3 to 25(OH)D3 and 1,25(OH)2D3. Once formed, 1,25(OH)2D3 carries out the biologic functions of vitamin D3 on the intestine and bone. Parathyroid hormone (PTH) promotes the synthesis of 1,25(OH)2D3, which, in turn, stimulates intestinal calcium transport, bone calcium mobilization and regulates the synthesis of PTH by negative feed back (9)
As can be seen in Figure 2.
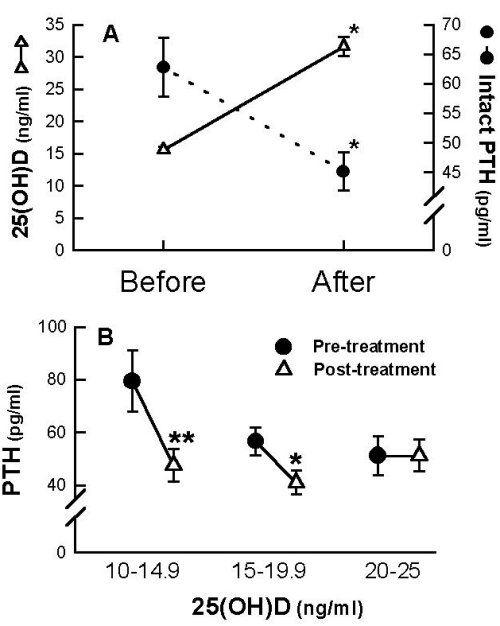 Fig. 2: (A) Serum levels of 25(OH)D (- -) and PTH (-· -) before and after therapy with 50,000 IU of vitamin D2 and calcium supplementation once a week for 8 weeks. (B) Serum levels of PTH levels in patients who had serum 25(OH)D levels of between 10 and 25 ng/ml and who were stratified in increments of 5 ng/ml before and after receiving 50,000 IU of vitamin D2 and calcium supplementation for 8 weeks *p<0.001,**p<0.02 (27)
Fig. 2: (A) Serum levels of 25(OH)D (- -) and PTH (-· -) before and after therapy with 50,000 IU of vitamin D2 and calcium supplementation once a week for 8 weeks. (B) Serum levels of PTH levels in patients who had serum 25(OH)D levels of between 10 and 25 ng/ml and who were stratified in increments of 5 ng/ml before and after receiving 50,000 IU of vitamin D2 and calcium supplementation for 8 weeks *p<0.001,**p<0.02 (27)
Recommended Adequate Dietary Intake of Vitamin D
Until 1997, the recommended dietary allowance for vitamin D for all adults was set at 200 IU a day. However, with compelling evidence that vitamin D deficiency is becoming a significant health problem especially for middle-aged and older adults, a panel for the Institute of Medicine (IOM) for the National Academy of Sciences reviewed whether this recommendation was adequate. Furthermore, they reviewed all of the literature on what was known about vitamin D impact on human health and disease from birth until death. The Institute of Medicine released in August 1997 their recommendations for vitamin D. They are as follows:
1. Birth to 1 year
After birth, infants only fed breast milk are prone to developing vitamin D deficiency especially during the winter (11-13). The reason for this is that human milk, as well as milk from other animals, does not contain significant amounts of vitamin D to satisfy the infant’s requirement. Infants at this age can synthesize vitamin D in their skin. It has been estimated at least in the mid-west that infants exposed to sunlight in the spring, summer, and fall require about 30 minutes a week (12). Vitamin D intakes between 340 and 600 IU/day have been reported to have maximal effects on linear growth in infants (14). However, since Chinese infants who were given 100, 200, or 400 IU of vitamin D a day did not demonstrate any evidence of rickets (13), and Markestad and Elzouki (11) reported in Norwegian infants fed infant formula containing 300 IU/day that the blood levels of 25(OH)D were above 11 ng/ml, which is considered to be the cut-off for vitamin D deficiency. Thus, based on the literature, it appeared tha t a minimum of 100 IU of vitamin D a day was satisfactory for preventing rickets. However, in the absence of any exposure to sunlight, it is probable that infants require a larger amount of vitamin D to optimize bone health. Thus, the IOM recommended as an adequate dietary intake for infants to be 200 IU/day. However, for infants not exposed to sunlight, the vitamin D intake should be at least 200 IU/day and to ensure that infants have a maximum amount of vitamin D required, the amount of 400 IU/day, the current amount included in one liter of standard infant formula or one quart of commercial cow’s milk, would not be excessive.
2. Ages 1 to 18 Years
Young and growing children require vitamin D for maximal skeleton development and mineralization. The fact that most children are outdoors and exposed to sunlight helps ensure that most children are not deficient in vitamin D (15-18). However, children with increased melanin pigmentation and who receive little sunlight either because they live in an inner city or are institutionalized, are at risk for vitamin D deficiency. Thus, the IOM recommended as a dietary intake for this age group 200 IU/day. However, in the absence of exposure to sunlight, it is reasonable to double this recommendation to 400 IU/day.
3. Ages 19-50
Most young and middle-aged adults are outdoors for recreational activities as well as their normal daily activities. There are very few studies that have evaluated the vitamin D requirement in this age group. An evaluation of 67 White and 70 Black premenopausal women ingesting 138 + 84 and 73 IU/day, respectively, revealed that serum 25(OH)D were in the low normal range at 21.4 + 12 and 18.3 + 9 ng/ml, respectively (19). However, in a group of young marine submariners who were not exposed to any sunlight for three months, a daily intake of 600 IU/day could not sustain circulating concentrations of 25(OH)D (1). Thus, based on cross sectional data and assuming some exposure to sunlight, the IOM recommended an adequate dietary intake for this age group to be 200 IU/day. However, 400 IU/day is not unreasonable and will not cause any adverse effects.
4. Ages 51 to 70 years
Men and women in this age group are very dependent on sunlight for most of their vitamin D requirement (20-23). However, this age group is much more health conscious and is especially concerned about their skin health as it relates to increased risk of skin cancer and wrinkles due to exposure to sunlight. The use of clothing on sun exposed areas and the topical application of sunscreen decreases or eliminates the ability of the skin to make vitamin D (1). There are several studies that have now provided convincing evidence that men and women in this age group require at least twice the amount of vitamin D compared to younger adults. Krall and Dawson-Hughes observed in healthy postmenopausal women (mean age 60 + 5 years), a seasonal variation in calcium retention that positively correlated with serum 25(OH)D levels in women on low calcium diets (20). Furthermore, an evaluation of bone loss in 247 postmenopausal women (mean 64 + 5 years), who consumed an average of 100 IU/day, found that women who received an additional supplement of 700 IU of vitamin D/day loss less bone then women who were on a total of 200 IU/day (21). These studies, as well as other studies, prompted the IOM to recommend for this age group that the adequate dietary intake be 400 IU/day. For those not exposed to sunlight, 600 IU of vitamin D/day is not inappropriate to maximize skeletal health.
5. Ages 71 and Older
This age group is especially at high risk for developing vitamin D deficiency and its consequences on the skeleton. This is due in part to the diminished capacity of their skin to make vitamin D and decreased activities outdoors. A multitude of studies that have evaluated dietary vitamin D supplementation in both men and women suggest that supplementation between 400 and 1000 units a day cause significant reduction in bone resorption (20,22,24). Of great importance is in a study of a group of elderly French woman who were supplemented with calcium and 800 IU of vitamin D; there was a significant increase of bone mineral content with a significant decrease in vertebral and non-vertebral fractures (25). A similar observation was made in free-living men and women 65 years and older who received 500 mg of calcium and 700 IU of vitamin D (26). Based on the recognition that vitamin D deficiency is a significant health problem for elderly throughout the industrialized world, the IOM recommended that the adequate dietary intake for this group should be three times the intake for younger adults or 600 IU/day. For those not exposed to any sunlight, they may need as much as 800 IU of vitamin D a day.
6. Pregnancy and Lactation.
Although intuitively one would assume that during pregnancy and lactation that due to the increase in calcium requirements for the mother, that there would be an increased requirement for a vitamin D. However, a careful review of the literature did not support this. Thus, the IOM recommended that an adequate intake for vitamin D during pregnancy and lactation be 200 IU/day. However, it is not unreasonable to double this amount to 400 IU/day, which is the amount supplied in prenatal supplements.
Tolerable Upper Intake Levels
The IOM reviewed the literature regarding vitamin D intake and intoxication. As noted in the Table, the safe upper level for infants to 12 months is 1000 IU of vitamin D/day. For children and adults, the recommended upper safe level was 2000 IU/day.
Conclusion
Vitamin D is taken for granted and not usually considered an important nutrient. Indeed, if adequate exposure of the skin to sunlight is available, vitamin D supplementation is not required. Since there are so many factors that can influence the cutaneous production of vitamin D, for example, in the winter no matter how much exposure to sunlight at certain latitudes will result in the production of vitamin D, it is reasonable to consider vitamin D as an essential nutrient. Vitamin D deficiency is now being recognized as a significant problem for adults over the age of 50 years (27-30). Two recent studies have suggested that between 40 and 60% of middle-aged and older adults are vitamin D insufficient (27,31). The consequence of vitamin D deficiency has been well described in this review. However, what is still not well understood is that there is an association with vitamin D deficiency and lack of exposure to sunlight as increasing risks for colon, breast and prostate cancer as well as osteoarthritis. Whe ther increasing vitamin D intake or exposure to sunlight will decrease these risks is unknown at this time. Clearly, maintenance of adequate vitamin D stores in the body from exposure to sunlight, dietary intake and supplementation would be a prudent course of action. The best way to treat vitamin D deficiency is to give 50,000 IU of vitamin D once a week for eight weeks followed by a multivitamin supplement that contains 400 IU of vitamin D (27)(Fig.2).
References
1. Holick, M.F. McCollum Award Lecture, 1994: Vitamin D: new horizons for the 21st century. Am J Clin Nutr 60:619-630, 1994.
2. Krane, S.M. and Holick, M.F. Metabolic bone disease. In: K.J. Isselbacher, E. Braunwald, J.D. Wilson et al (eds.) Harrison's Principles of Internal Medicine, 13th Edition. New York: McGraw-Hill, Inc., pp. 2172-2183, 1994.
3. Clemens, T.L., Henderson, S.L., Adams, J.S., and Holick, M.F. Increased skin pigment reduces the capacity of skin to synthesize vitamin D3. Lancet, 74-76, 1982.
4. Matsuoka, L.Y., Ide, L., Wortsman, J., MacLaughlin, J., and Holick, M.F. Sunscreens suppress cutaneous vitamin D3 synthesis. J. Clin. Endocrinol. Metab. 64: 1165-1168, 1987.
5. Holick, M.F., Matsuoka, L.Y., and Wortsman, J. Age, Vitamin D, and solar ultraviolet radiation. Lancet, November 4: 1104-1105, 1989.
6. Webb, A.R., Kline, L., and Holick, M.F. Influence of season and latitude on the cutaneous synthesis of vitamin D3: Exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J. Clin. Endocrinol. Metab. 67: 373-378, 1988.
7. Holick, M.F., Shao, Q., Liu, W.W., and Chen, T.C. The vitamin D content of fortified milk and infant formula. N. Engl. J. Med. 326: 1178-1181, 1992.
8. Holick, M.F. Vitamin D: Photobiology, Metabolism, and Clinical Applications. In: L. DeGroot, et al. (eds.) Endocrinology, 3rd Edition, Chapter 59. Philadelphia:W.B. Saunders, pp. 990-1013, 1995.
9. Holick, M.F. Vitamin D: photobiology, metabolism, mechanism of action, and clinical application. In: M.J. Favus (ed.) Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, Third Edition, pp. 74-8l, Lippincott-Raven: Philadelphia, 1996.
10. Strugnell, S.A. and DeLuca, H.F. The vitamin D receptor--structure and transcriptional activation. Proc. Soc. Exp. Bio. Med. 215: 223-228, 1997.
11. Markestad, T. and Elzouki, A.Y. Vitamin D deficiency rickets in northern Europe and Libya. In: F.H. Glorieux (ed.), Rickets Nestle Nutrition Workshop Series, pp. 203-213, New York: Raven Press,1991.
12. Specker, B.L., Valanis, B., Hertzberg, V., Edwards, N., and Tsang, R.C. Sunshine exposure and serum 25-hydroxyvitamin D. J. Pediatr. 107: 372-376, 1985.
13. Specker, B.L. and Tsang, R.C. Cyclical serum 25-hydroxyvitamin D concentrations paralleling sunshine exposure in exclusively breast-fed infants. J. Pediatr. 110: 744-747, 1987.
14. Foman SJ, Younoszai K, and Thomas L. Influence of vitamin D on linear growth of normal full-term infants. J. Nutr. 88:345-350, 1966.
15. Pettifor, J.M., Ross, F.P., Moodley, G., Wang, J., and et al. Serum calcium, magnesium, phosphorus, alkaline, phosphatase and 25-hydroxyvitamin D concentrations in children. A. Afr. Med. J. 53: 751-754, 1978.
16. Aksnes, L. and Aarskog, D. Plasma concentrations of vitamin D metabolites in puberty: effect of sexual maturation and implications for growth. J. Clin. Endocrinol. Metab. 55: 94-101, 1982.
17. Gultekin, A., Ozalp, I., Hasanoglu, A., and Unal, A. Serum-25-hydroxycholecalciferol levels in children and adolescents. Turkish J. Pediatr. 29: 155-162, 1987.
18. Riancho, J.A., del Arco, C., Arteaga, R., Herranz, J.L., Albajar, M., Macias, J.G. Influence of solar irradiation on vitamin D levels in children on anticonvulsant drugs. Acta Neurol. Scand. 79:296-299,1989.
19. Meier, D.E., Luckey, M.M., Wallenstein, S., Clemens, T.L., et al. Calcium, vitamin D, and parathyroid hormone status in young white and black women: Association with racial differences in bone mass. J. Clin. Endocrinol. Metab. 72:703-710, 1991.
20. Krall, E.A. and Dawson-Hughes, B. Relation of fractional 47Ca retention to season and rates of bone loss in healthy postmenopausal women. J. Bone Min. Res. 6: 1323-1329, 1991.
21. Dawson-Hughes, B., Harris, S.S., Krall, E.A., Dallal, G.E., Falconer, G., and Green, C.L. Rates of bone loss in postmenopausal women randomly assigned to one of two dosages of vitamin D. Am. J. Clin. Nutr. 61: 1140-1145, 1995.
22. Dawson-Hughes, B., Dallal, G.E., Krall, E.A., Harris, S., Sokoll, L.J., and Falconer, G. Effect of vitamin D supplementation on wintertime and overall bone loss in healthy postmenopausal women. Annals of Int. Med. 115: 505-512, 1991.
23. Webb, A.R., Pilbeam, C., Hanafin, N., and Holick, M.F. An evaluation of the relative contributions of exposure to sunlight and diet on the circulating concentrations of 25-hydroxyvitamin D in an elderly nursing home population in Boston. Am. J. Clin. Nutr. 51:1075-1081, 1990.
24. Krall, E., Sahyoun, N., Tannenbaum, S., Dallal, G., and Dawson-Hughes, B. Effect of vitamin D intake on seasonal variations in parathyroid hormone secretion in postmenopausal women. N. Engl. J. Med. 321: 1777-1783, 1989.
25. Chapuy, M.C., Arlot, M., Duboeuf, F., Brun, J., Crouzet, B., Arnaud, S., Delmas, P., and Meuner, P. Vitamin D3 and calcium to prevent hip fractures in elderly women. N. Engl. J. Med. 327: 1637-1642, 1992.
26. Dawson-Hughes, B., Harris, S.S., Krall, E.A., and Dallal, G.E. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N. Engl. J. Med. 337: 670-676, 1997.
27. Malabanan, A., Veronikis, I.E., and Holick, M.F. Redefining vitamin D deficiency. Lancet 351: 805-806, 1998.
28. Lamberg-Allardt, C., Karkkainen, M., Seppanen, R., and Bistrom, H. Low serum 25-hydroxyvitamin D concentrations and secondary hyperparathyroidism in middle-aged white strict vegetarians. Am. J. Clin. Nutr. 58: 684-689, 1993.
29. Lips, Wiersinga, A., van Ginkel, F.C., Jongen, M.J.M., Netelenbos, C., Hackeng, W.H.L., and et al. The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J. Clin. Endocrinol. Metab. 67: 644-650, 1988.
30. Villareal, D.T., Civitelli, R., Chines, A., and Avioli, L.V. Subclinical vitamin D deficiency in postmenopausal women with low vertebral bone mass. J. Clin. Endocrinol. Metab. 72: 628-634, 1991.
31. Thomas, M.K., Lloyd-Jones, D.M., Thadhani, R.I., Shaw, A.C., Deraska, D.J., Kitch, B.T., Vamvakas, E.C., Dick, I.M., Prince, R.L., and Finkelstein, J.S. Hypovitaminosis D in medical inpatients. N. Engl. J. Med. 338: 777-783, 1998.
| Discussion Board | Previous Page | Your Symposium |